In this nationally representative cross-sectional study, we found that higher LE8 scores was associated with a lower prevalence of periodontitis. Participants with moderate (50–79) and high (80–100) LE8 scores had 58% and 55% lower odds of periodontitis, respectively, compared with participants with lower (0–49) LE8 scores, after adjusting for potential confounders. Among the LE8 components, nicotine exposure, blood glucose, sleep heath, and blood pressure significantly impacted periodontitis. In addition, systemic inflammation, as evidenced by levels of neutrophils, white blood cells, and albumin, emerged as a mediator linking LE8 to periodontitis. To our knowledge, this is one of the few studies to demonstrate study demonstrating an inverse association between the AHA’s new cardiovascular health metric LE8 and periodontitis in US adults.
Our findings are consistent with previous studies showing that ideal cardiovascular health is associated with lower risks of periodontitis17,18. Several potential mechanisms may explain the observed association between better cardiovascular health and lower periodontitis prevalence. First, cardiovascular diseases and periodontitis share common risk factors, such as smoking19, diabetes20, and physical inactivity21. Second, chronic inflammation plays a vital role in the pathogenesis of both atherosclerotic cardiovascular disease9 and periodontitis10. Third, our mediation analysis provided evidence supporting systemic inflammation as an intermediate pathway linking cardiovascular health to periodontitis.
Our findings show that the higher the LE8 score, the lower the prevalence of periodontitis. Our results align with the evidence linking LE8 to lower incidences of atherosclerotic cardiovascular disease, cancer, diabetes, and all-cause mortality6,7,22. The observed inverse association between LE8 and periodontitis prevalence also corroborates prior research indicating the detrimental impacts of unfavorable lifestyle factors such as smoking, obesity, hypertension, and diabetes on periodontal health19,23,24,25.
Furthermore, the mediating role of systemic inflammation found in our study is consistent with the current understanding of the pathogenesis of both cardiovascular disease and periodontitis9,10,26. Several potential biological mechanisms may explain the observed inverse association between cardiovascular health and periodontitis. First, chronic inflammation plays a vital role in the pathogenesis of both cardiovascular disease and periodontitis26,27. Elevated levels of inflammatory biomarkers have been linked to increased risks of atherosclerosis, myocardial infarction and stroke28. Meanwhile, the inflammatory response induced by periodontal bacteria is recognized as the primary pathway leading to the destruction of periodontal tissues. Our study provides novel evidence that systemic inflammation may be a common pathway through which cardiovascular health influences periodontitis. However, in our analysis, we found that CRP did not mediate the relationship between LE8 and periodontitis. The data for CRP were significantly missing from the NHANES database, therefore, we believe that the representativeness and statistical validity of the study results may be reduced due to objective factors such as missing data. Meanwhile, due to uncontrollable factors such as missing data and sample representativeness issues, we were not able to include fibrinogen, interleukins, and TNF- α, which are more representative of systemic inflammation, and therefore the results may not fully reflect the role of inflammation in periodontal disease. To elucidate the intricate interactions between cardiovascular health, inflammation, and periodontitis, it is necessary to consider and discuss these important biomarkers more comprehensively in future studies in order to provide more complete and accurate results.
Second, metabolic disorders like diabetes can increase susceptibility to periodontitis29,30. Hyperglycemia impairs neutrophil function and collagen synthesis, resulting in more severe periodontal breakdown31. The glycemic control component in LE8 is associated with diabetes risk, which may subsequently influence periodontitis risk.
Third, smoking is a major modifiable risk factor for both cardiovascular disease and periodontitis32. Tobacco smoke induces systemic inflammation and endothelial dysfunction, which can exacerbate both atherosclerosis and periodontal tissue destruction. The nicotine exposure metric in LE8 captures the adverse impacts of smoking on oral and cardiovascular health. Tobacco/nicotine exposure was confirmed as a strong predictor of periodontitis in the WQS index-related results, which not only validates existing research findings but also emphasizes the importance of controlling tobacco exposure in health management and prevention strategies.
In contrast, BMI and physical activity were given less weight in the WQS index correlation results. We consider the possibility that on the one hand, our sample, which contained a larger number of individuals with normal or near-normal BMI, had relatively little variability and thus lacked sufficient differences to affect the predictive power of the model significantly. In addition, BMI and physical activity are influenced by other factors, which may also result in their effect on periodontitis being masked by other, more direct risk factors. The mechanisms by which BMI and physical activity influence periodontitis are more complex, and it is possible that these factors may have a greater influence on the overall assessment of health, thus reducing their independent contribution.
In summary, the potential mechanisms linking LE8 to periodontitis appear to be multifactorial, involving shared risk factors, chronic inflammation, metabolic disorders, and unhealthy lifestyles like smoking. Further research is needed to elucidate the complex interactions better.
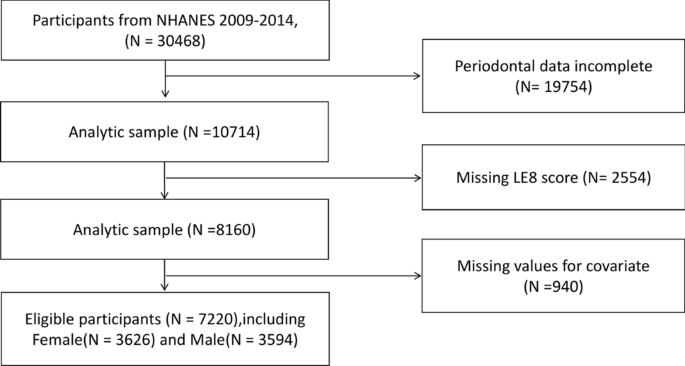
Our study has several notable strengths. First, few previous studies have explored the relationship between LE8 and periodontitis, our study adds novel evidence to the literature. Second, our analysis was based on a large nationally representative sample of US adults, enhancing the external validity and generalizability of the findings. Third, using the LE8 provides a comprehensive assessment of lifestyle habits by combining smoking, body mass index, diet, physical activity, cholesterol, blood glucose, and blood pressure. Not only does it focus on the direct impact of individual risk factors on periodontal disease, but it also examines the potential interactions between these factors. This integrated perspective provides a more comprehensive assessment of health status than a single risk factor analysis, and a more precise identification of high-risk populations, thus providing an important basis for early intervention and prevention. As a result, risk estimates are more reliable than in previous studies of individual factors. The LE8 Index, a comprehensive health assessment tool, highlights the potential effectiveness of reducing the incidence of periodontal disease through overall health behavior improvement. This provides a new way of thinking about public health strategies, whereby broader health gains can be realized by promoting a holistic healthy lifestyle, rather than just controlling individual risk factors.
However, some limitations should be acknowledged. First, the cross-sectional nature precludes causal inference, and the possibility of reverse causation cannot be ruled out. Prospective cohort studies are warranted to determine the temporal sequence between LE8 and periodontitis. Second, LE8 scores were calculated primarily based on self-reported data, possibly subject to recall bias. Future research should include more objective measurements, such as accelerometers for physical activity. In addition, some indicators that are more responsive to systemic inflammation could not be included in the analysis due to uncontrollable factors such as missing data. Nevertheless, our study provides novel and valuable insights into the relationship between ideal lifestyle habits and lower periodontitis prevalence in US adults. Further intervention studies are needed to verify whether improving lifestyle habits reduces the risk of periodontitis.
The study provides evidence that improving lifestyle habits may confer benefits in preventing periodontitis. Periodontitis is a highly prevalent chronic inflammatory disease that affects nearly half of US adults2. Our results suggest that promoting cardiovascular health through lifestyle changes and risk factor control could be a promising population-based strategy to curb the rising burden of periodontitis. The LE8 score provides a framework for integrated health management that can help clinicians comprehensively assess a patient’s overall health status, contributing to the development of more holistic prevention and treatment strategies as well as individualized interventions to improve a patient’s overall health. At the same time, through early identification and management of multiple health risk factors, the LE8 can help reduce the incidence of periodontitis and the healthcare burden and costs associated with it.
The association between better lifestyle habits and lower periodontitis prevalence warrants further investigation in prospective cohort studies to determine causal relationships and temporal sequence33. Future research should also explore whether incorporating periodontal disease prevention and treatment into CVH management programs can improve oral and systemic health outcomes. Community-based interventions targeting shared modifiable risk factors may be a practical approach to managing both cardiovascular disease and periodontitis34.