Jardim, S. R., de Souza, L. M. P. & de Souza, H. S. P. The rise of gastrointestinal cancers as a global phenomenon: unhealthy behavior or progress? Int. J. Environ. Res. Public. Health 20. https://doi.org/10.3390/ijerph20043640 (2023).
Wang, S. et al. Global, regional, and national lifetime risks of developing and dying from gastrointestinal cancers in 185 countries: a population-based systematic analysis of GLOBOCAN. Lancet Gastroenterol. Hepatol. 9, 229–237. https://doi.org/10.1016/s2468-1253(23)00366-7 (2024).
Vernia, F., Longo, S., Stefanelli, G., Viscido, A. & Latella, G. Dietary factors modulating colorectal carcinogenesis. Nutrients 13. https://doi.org/10.3390/nu13010143 (2021).
Keum, N. & Giovannucci, E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 16, 713–732. https://doi.org/10.1038/s41575-019-0189-8 (2019).
Fund, W. C. R. & Research (2018). A. I. o. C.
Farvid, M. S. et al. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 36, 937–951. https://doi.org/10.1007/s10654-021-00741-9 (2021).
Aune, D. et al. Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Annals Oncology: Official J. Eur. Soc. Med. Oncol. 23, 37–45. https://doi.org/10.1093/annonc/mdr269 (2012).
Ma, Y. et al. Dietary fiber intake and risks of proximal and distal colon cancers: a meta-analysis. Medicine 97, e11678. https://doi.org/10.1097/md.0000000000011678 (2018).
Tangestani, H., Salari-Moghaddam, A., Ghalandari, H. & Emamat, H. Adherence to the Dietary approaches to stop hypertension (DASH) dietary pattern reduces the risk of colorectal cancer: a systematic review and meta-analysis. Clin. Nutr. 39, 2975–2981. https://doi.org/10.1016/j.clnu.2020.02.002 (2020).
Sharma, I. et al. Inflammatory diet and risk for colorectal cancer: a population-based case-control study in Newfoundland. Can. Nutr. 42, 69–74. https://doi.org/10.1016/j.nut.2017.05.010 (2017).
Hu, F. B. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13, 3–9. https://doi.org/10.1097/00041433-200202000-00002 (2002).
Nestel, P. J., Beilin, L. J. & Mori, T. A. Changing dietary approaches to prevent cardiovascular disease. Curr. Opin. Lipidol. 31, 313–323. https://doi.org/10.1097/mol.0000000000000709 (2020).
Schwingshackl, L., Schwedhelm, C., Galbete, C. & Hoffmann, G. Adherence to Mediterranean Diet and Risk of Cancer: an updated systematic review and Meta-analysis. Nutrients 9. https://doi.org/10.3390/nu9101063 (2017).
Steck, S. E., Guinter, M., Zheng, J. & Thomson, C. A. Index-based dietary patterns and colorectal cancer risk: a systematic review. Adv. Nutr. 6, 763–773. https://doi.org/10.3945/an.115.009746 (2015).
Li, W. Q. et al. Index-based dietary patterns and risk of esophageal and gastric cancer in a large cohort study. Clin. Gastroenterol. Hepatology: Official Clin. Pract. J. Am. Gastroenterological Association 11, 1130–1136e1132. https://doi.org/10.1016/j.cgh.2013.03.023 (2013).
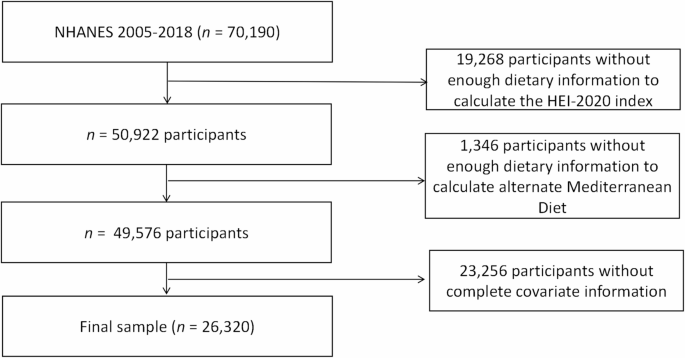
Luo, T. & Tseng, T. S. Diet quality as assessed by the healthy eating index-2020 among different smoking status: an analysis of national health and nutrition examination survey (NHANES) data from 2005 to 2018. BMC Public. Health 24, 1212. https://doi.org/10.1186/s12889-024-18630-7 (2024).
Krebs-Smith, S. M. et al. Update of the healthy eating index: HEI-2015. J. Acad. Nutr. Diet. 118, 1591–1602. https://doi.org/10.1016/j.jand.2018.05.021 (2018).
Mentella, M. C., Scaldaferri, F., Ricci, C., Gasbarrini, A. & Miggiano, G. A. D. Cancer and Mediterranean Diet: a review. Nutrients 11. https://doi.org/10.3390/nu11092059 (2019).
Farinetti, A., Zurlo, V., Manenti, A., Coppi, F. & Mattioli, A. V. Mediterranean diet and colorectal cancer: a systematic review. Nutrition 43–44, 83–88. https://doi.org/10.1016/j.nut.2017.06.008 (2017).
Yammine, A. et al. Polyphenols of the Mediterranean Diet and their metabolites in the Prevention of Colorectal Cancer. Molecules 26. https://doi.org/10.3390/molecules26123483 (2021).
Wang, Y., Fan, H., Ren, Z., Liu, X. & Niu, X. Sleep disorder, Mediterranean diet, and all-cause and cause-specific mortality: a prospective cohort study. BMC Public. Health 23, 904. https://doi.org/10.1186/s12889-023-15870-x (2023).
Sautin, Y. Y. & Johnson, R. J. Uric acid: the oxidant-antioxidant paradox. Nucleosides Nucleotides Nucleic Acids 27, 608–619. https://doi.org/10.1080/15257770802138558 (2008).
Kanellis, J. & Kang, D. H. Uric acid as a mediator of endothelial dysfunction, inflammation, and vascular disease. Semin Nephrol. 25, 39–42. https://doi.org/10.1016/j.semnephrol.2004.09.007 (2005).
Choi, H. K. & Curhan, G. Gout: epidemiology and lifestyle choices. Curr. Opin. Rheumatol. 17, 341–345 (2005).
Don, B. R. & Kaysen, G. Serum albumin: relationship to inflammation and nutrition. Semin. Dial. 17, 432–437. https://doi.org/10.1111/j.0894-0959.2004.17603.x (2004).
Gupta, D. & Lis, C. G. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr. J. 9, 69. https://doi.org/10.1186/1475-2891-9-69 (2010).
Kuczmarski, M. F. & Weddle, D. O. Position paper of the American Dietetic Association: nutrition across the spectrum of aging. J. Am. Diet. Assoc. 105, 616–633. https://doi.org/10.1016/j.jada.2005.02.026 (2005).
Estruch, R. et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet supplemented with Extra-virgin Olive oil or nuts. N Engl. J. Med. 378, e34. https://doi.org/10.1056/NEJMoa1800389 (2018).
Fan, Y. et al. Non-linear association between Mediterranean diet and depressive symptom in U.S. adults: a cross-sectional study. Front. Psychiatry. 13, 936283. https://doi.org/10.3389/fpsyt.2022.936283 (2022).
Fung, T. T. et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 82, 163–173. https://doi.org/10.1093/ajcn.82.1.163 (2005).
Powell-Wiley, T. M. et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 143, e984–e1010. https://doi.org/10.1161/cir.0000000000000973 (2021).
Yeom, H. E. & Lee, J. The association of education level with autonomy support, self-efficacy and health behaviour in patients with cardiovascular risk factors. J. Clin. Nurs. 31, 1547–1556. https://doi.org/10.1111/jocn.16008 (2022).
Odutayo, A. et al. Income disparities in Absolute Cardiovascular Risk and Cardiovascular Risk factors in the United States, 1999–2014. JAMA Cardiol. 2, 782–790. https://doi.org/10.1001/jamacardio.2017.1658 (2017).
Chang, Y., Yu, C., Dai, X., Sun, H. & Tang, T. Association of dietary inflammatory index and dietary oxidative balance score with gastrointestinal cancers in NHANES 2005–2018. BMC Public. Health 24, 2760. https://doi.org/10.1186/s12889-024-20268-4 (2024).
Wang, X. et al. Association of dietary inflammatory potential, dietary oxidative balance score and biological aging. Clin. Nutr. 43, 1–10. https://doi.org/10.1016/j.clnu.2023.11.007 (2024).
Qiu, X., Sun, X., Li, H. O., Wang, D. H. & Zhang, S. M. Maternal alcohol consumption and risk of postpartum depression: a meta-analysis of cohort studies. Public. Health 213, 163–170. https://doi.org/10.1016/j.puhe.2022.08.020 (2022).
Plante, T. B. et al. Life’s simple 7 and Incident Hypertension: the REGARDS Study. J. Am. Heart Association. 9, e016482. https://doi.org/10.1161/jaha.120.016482 (2020).
Diagnosis and classification of diabetes mellitus. Diabetes care 34(Suppl 1), 62–69. https://doi.org/10.2337/dc11-S062 (2011).
Buckland, G. et al. Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European prospective investigation into Cancer and Nutrition (EPIC) cohort study. Am. J. Clin. Nutr. 91, 381–390. https://doi.org/10.3945/ajcn.2009.28209 (2010).
Moazzen, S., van der Sloot, K. W. J., Vonk, R. J., de Bock, G. H. & Alizadeh, B. Z. Diet Quality and Upper gastrointestinal cancers risk: a Meta-analysis and critical Assessment of evidence quality. Nutrients 12. https://doi.org/10.3390/nu12061863 (2020).
La Vecchia, C. & Bosetti, C. Diet and cancer risk in Mediterranean countries: open issues. Public. Health Nutr. 9, 1077–1082. https://doi.org/10.1017/s1368980007668475 (2006).
Morze, J. et al. An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer. Eur. J. Nutr. 60, 1561–1586. https://doi.org/10.1007/s00394-020-02346-6 (2021).
Julián-Serrano, S., Reedy, J., Robien, K. & Stolzenberg-Solomon, R. Adherence to 5 Diet Quality indices and Pancreatic Cancer Risk in a large US prospective cohort. Am. J. Epidemiol. 191, 1584–1600. https://doi.org/10.1093/aje/kwac082 (2022).
Valko, M., Rhodes, C. J., Moncol, J., Izakovic, M. & Mazur, M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem. Biol. Interact. 160, 1–40. https://doi.org/10.1016/j.cbi.2005.12.009 (2006).
Aggarwal, B. B. & Sung, B. Pharmacological basis for the role of curcumin in chronic diseases: an age-old spice with modern targets. Trends Pharmacol. Sci. 30, 85–94. https://doi.org/10.1016/j.tips.2008.11.002 (2009).
Chan, D. S. et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PloS One 6, e20456. https://doi.org/10.1371/journal.pone.0020456 (2011).
Eichelmann, F., Schwingshackl, L., Fedirko, V. & Aleksandrova, K. Effect of plant-based diets on obesity-related inflammatory profiles: a systematic review and meta-analysis of intervention trials. Obes. Rev. 17, 1067–1079. https://doi.org/10.1111/obr.12439 (2016).
Bastide, N. M., Pierre, F. H. & Corpet, D. E. Heme iron from meat and risk of colorectal cancer: a meta-analysis and a review of the mechanisms involved. Cancer Prev. Res. (Phila) 4, 177–184. https://doi.org/10.1158/1940-6207.Capr-10-0113 (2011).
Reedy, J. et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J. Nutr. 144, 881–889. https://doi.org/10.3945/jn.113.189407 (2014).
Sofi, F., Abbate, R., Gensini, G. F. & Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am. J. Clin. Nutr. 92, 1189–1196. https://doi.org/10.3945/ajcn.2010.29673 (2010).
Zhu, Y., Pandya, B. J. & Choi, H. K. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 63, 3136–3141. https://doi.org/10.1002/art.30520 (2011).
Jiang, M., Ren, L., Chen, S. & Li, G. Serum uric acid levels and risk of eight site-specific cancers: a mendelian randomization study. Front. Genet. 12, 608311. https://doi.org/10.3389/fgene.2021.608311 (2021).
Sautin, Y. Y., Nakagawa, T., Zharikov, S. & Johnson, R. J. Adverse effects of the classic antioxidant uric acid in adipocytes: NADPH oxidase-mediated oxidative/nitrosative stress. Am. J. Physiol. Cell. Physiol. 293, C584–596. https://doi.org/10.1152/ajpcell.00600.2006 (2007).
Allegra, A., Caserta, S., Genovese, S., Pioggia, G. & Gangemi, S. Gender differences in oxidative stress in relation to Cancer susceptibility and survival. Antioxid. (Basel Switzerland) 12. https://doi.org/10.3390/antiox12061255 (2023).
Tiberi, J. et al. Sex differences in antioxidant defence and the regulation of redox homeostasis in physiology and pathology. Mech. Ageing Dev. 211, 111802. https://doi.org/10.1016/j.mad.2023.111802 (2023).
Kim, S. Y. Oxidative stress and gender disparity in cancer. Free Radic. Res. 56, 90–105. https://doi.org/10.1080/10715762.2022.2038789 (2022).
Shams-White, M. M. et al. Healthy eating Index-2020: review and update process to reflect the Dietary guidelines for Americans,2020–2025. J. Acad. Nutr. Diet. 123, 1280–1288. https://doi.org/10.1016/j.jand.2023.05.015 (2023).
Stote, K. S., Radecki, S. V., Moshfegh, A. J., Ingwersen, L. A. & Baer, D. J. The number of 24 h dietary recalls using the US Department of Agriculture’s automated multiple-pass method required to estimate nutrient intake in overweight and obese adults. Public Health. Nutr. 14, 1736–1742. https://doi.org/10.1017/s1368980011000358 (2011).
Ahluwalia, N., Dwyer, J., Terry, A., Moshfegh, A. & Johnson, C. Update on NHANES Dietary Data: Focus on Collection, Release, Analytical considerations, and uses to inform Public Policy. Adv. Nutr. 7, 121–134. https://doi.org/10.3945/an.115.009258 (2016).
Fanelli Kuczmarski, M. et al. Aspects of Dietary Diversity Differ in Their Association with Atherosclerotic Cardiovascular Risk in a racially diverse US Adult Population. Nutrients 11. https://doi.org/10.3390/nu11051034 (2019).
Jun, S. et al. Association of food insecurity with dietary intakes and nutritional biomarkers among US children, National Health and Nutrition Examination Survey (NHANES) 2011–2016. Am. J. Clin. Nutr. 114, 1059–1069. https://doi.org/10.1093/ajcn/nqab113 (2021).