Statement of principal findings
This study aimed to identify the factors associated with healthy lifestyle behaviors in older adults with diabetes, adopting a socioecological model as a theoretical framework. The study demonstrated significant disparities in the health profiles of the five lifestyles: sleep, diet, physical activity, drinking, and smoking. Notably, sleep emerged as a major health risk, with only 14.71% of individuals demonstrating healthy sleep habits. In addition, our conclusions indicate that the influencing factors are primarily centered around four levels: Individual Characteristics, Individual Behaviors, Community, and Policy. We think that the policymakers should prioritize these modifiable factors, thoroughly examining their impact, and proposing practicable policy recommendations based on our findings. Here are our thoughts on the article.
Prioritize Sleep health and develop targeted policies for health promotion
Insufficient sleep is associated with an increased risk of developing numerous chronic diseases, which has a profoundly detrimental impact on health15. Globally, especially in developing countries, sleep is rarely addressed in the public health agenda at the national level16. An increasing number of older adults are facing sleep deprivation. Some studies have recommended that middle-aged and older adults improve sleep quality through interventions such as increased light hours, physical activities, and cognitive behavioral therapy17.
Public health organizations should prioritize sleep health by incorporating relevant research recommendations into targeted promotional and educational policies for healthy sleep. Effective strategies include implementing health talks and community education programs to promote sleep health awareness, leveraging telemedicine and mobile health tools to provide convenient sleep monitoring and consultation, and introducing cost-effective psychological interventions such as Cognitive Behavioral Therapy could be highly effective. Additionally, integrating sleep health into national public health policies, with tailored intervention plans and financial support for rural older adults, is strongly recommended. These measures have the potential not only to improve sleep health among rural older adults with diabetes significantly but also to enhance glycemic control and overall health outcomes.
Gender differences and cognitive competence in healthy lifestyle behaviors among older adults with diabetes
At the Individual Characteristics, sex was identified as a significant factor influencing the HLS among older adults with diabetes. Previous studies have demonstrated that gender differences in body structure lead to variations in bodily functions and lifestyle choices over the course of an individual’s life18. For instance, differences in body structure result in notable variations in sleep patterns between males and females, with females generally experiencing poorer sleep quality19. Regarding dietary habits, males and females differ in food choices, eating behaviors, and nutritional strategies20. Females are more likely to follow nutritionally balanced diets and prefer healthy, low-fat foods, whereas males tend to consume foods rich in sugar and fats. Physical activity levels also differ significantly, with females typically engaging in less frequent and lower-intensity exercise compared to males. In terms of alcohol consumption, females not only consume less alcohol but also represent a smaller proportion of drinkers compared to males. Furthermore, females find it easier to quit drinking if they do consume alcohol21. Similarly, while smoking prevalence is lower among females in rural areas, women are generally more successful at reducing or quitting smoking compared to men22.
Cognitive competence also emerged as an important determinant of HLS. Studies have confirmed a positive association between healthy lifestyles and cognitive function in the older adults, with evidence suggesting a bidirectional relationship23. Healthy lifestyles serve as an essential non-medical intervention, playing a vital role in maintaining cognitive function in older adults24. In contrast, HLS was lower among individuals with diabetic complications. Healthy lifestyles not only help prevent type 2 diabetes (T2D) but also significantly reduce the risk of associated complications25,26,27. This suggests a reciprocal relationship between diabetic complications and lifestyle behaviors, where one can influence the other. Therefore, it is essential to promote the importance of adopting healthy lifestyles as part of diabetes prevention and management strategies to reduce the likelihood of complications.
Given the distinct lifestyle preferences and barriers faced by men and women, designing tailored interventions that address these unique needs is crucial for managing diabetes and mitigating cognitive decline. For instance, interventions targeting women can emphasize healthy dietary practices, leveraging community lectures and online courses to promote the Mediterranean diet. These initiatives can encourage the consumption of dark leafy vegetables, nuts, and fish, which are rich in antioxidants and omega-3 fatty acids, while also offering subsidies for healthy food purchases. In contrast, interventions for men can focus on physical activity, particularly through the establishment of strength training and high-intensity interval training (HIIT) programs at community centers or workplaces. Providing free or low-cost access to fitness facilities can further enhance adherence to these exercise regimens. Such gender-specific strategies not only align with the preferences and challenges of each group but also offer a more effective approach to addressing the dual challenges of diabetes management and cognitive health.
Focus on modifiable behaviors: reducing depression and enhancing social engagement
At the Individual Behaviors, the study revealed that individuals with depression had lower HLS, which may lead to unhealthy lifestyle patterns. Several factors could explain this finding. First, people with depression often experience shorter sleep durations, resulting in poorer sleep quality28. Second, depression is associated with a stronger preference for sweets, irregular eating habits, and overeating29,30. Third, individuals with depression are more likely to smoke, and their success rate for quitting smoking is significantly lower compared to smokers in the general population31,32. Fourth, research indicates that individuals with higher subjective well-being are more likely to engage in physical activity33. In contrast, those with depression, who tend to have lower subjective well-being, often lack the motivation and initiative to participate in physical activities and may engage in such activities less frequently or at lower intensity. Extensive research has demonstrated that maintaining healthy lifestyles effectively reduces the risk of depression. A positive association exists between healthy lifestyles and depression, with each influencing the other.
Public health policies for diabetes prevention and control should prioritize addressing the needs of individuals with depression. Tailored interventions that promote and guide healthy lifestyle behaviors for this population could help alleviate the dual burden of depression and diabetes. In rural areas, the challenges of addressing depression are compounded by geographic isolation, socioeconomic disparities, and a lack of specialized mental health resources. Community-based interventions could play a crucial role in bridging these gaps by providing accessible and culturally appropriate support. For example, telehealth services could offer remote counseling and therapy, overcoming barriers related to distance and transportation. Peer support groups, facilitated by trained volunteers or healthcare professionals, could provide a sense of community and reduce feelings of isolation. Additionally, integrating mental health services into primary care settings could ensure that individuals receive comprehensive care, with early identification and treatment of depression becoming an integral part of routine medical visits.
This study also confirmed that higher levels of social engagement were positively associated with higher HLS in older adults with diabetes. Social engagement is a vital indicator of physical and mental health in older adults and forms the foundation of active aging. It supports the development of healthy lifestyle behaviors, and adherence to such behaviors can be enhanced through initiatives that increase social participation among residents34. For instance, older adults with higher social engagement levels tend to have better sleep quality35. Ecological-level interventions may help physically inactive seniors by leveraging social activities and interpersonal relationships to encourage greater participation in physical activities. Furthermore, higher levels of social engagement are strongly associated with improved cognitive abilities. Enhancing and protecting cognitive competence can enable older adults to maintain healthier lifestyles36. Enhancing social participation among older adults benefits individuals, their families, and society as a whole, fostering long-term commitment to healthy lifestyle behaviors37. Public health institutions should recognize the importance of promoting social engagement and develop programs that enrich the content and forms of social activities for older adults to foster active aging and holistic well-being38.
Leveraging community and policy strategies to improve lifestyle choices and health outcomes
At the community level, we also found that HLS was associated with occupation, income, and transportation. These findings are consistent with previous research indicating that socioeconomic status, which encompasses education, occupation, and income, significantly shapes lifestyle choices39. Socioeconomic status has a profound impact on physical health, with lifestyle often acting as a mediator between socioeconomic factors and health outcomes. Studies suggest that socioeconomic conditions near the workplace can influence individuals’ health behaviors40. For example, a study in the United States assessed how smoking, alcohol consumption, and physical inactivity moderated the relationship between socioeconomic status and all-cause mortality, highlighting the intricate connections between these variables41. Socioeconomic status and lifestyle behaviors thus form an interdependent relationship that warrants continued investigation.
At the policy level, this study revealed that HLS was significantly associated with the type of health insurance, with insurance choices ultimately shaping both lifestyle behaviors and overall health. First, different types of medical insurance vary in their protection and coverage scopes, which may impact patients’ access to and utilization of medical resources, and subsequently influence their health management awareness and behaviors. Second, the type of medical insurance may also indirectly affect patients’ lifestyle choices by influencing their economic burdens. In addition, research on orthopedic patients has shown that insurance type can influence health outcomes, such as recovery and reported quality of life42. Similarly, studies on patients using left ventricular assist devices (LVADs) found that payer type was linked to the incidence of adverse events, with medical insurance patients experiencing higher rates compared to those with commercial insurance43. Another study in the United States examined the impact of health insurance status and type on blood pressure control in women, emphasizing the critical role of insurance in managing chronic conditions like hypertension.
In summary, the community should formulate distinct lifestyle promotion strategies based on occupational traits. It should conduct health training for agricultural workers covering diabetes prevention, diet, and exercise knowledge. For non-agricultural workers, the community should offer health services and organize activities to boost social participation. Regarding low-income groups, while the government refines the medical assistance policy, the community helps identify and register eligible elderly diabetic patients, organizes volunteers to assist with daily needs like shopping for healthy food and accompanying them to medical appointments, and alleviates their life stress to focus on health. In medical insurance, as the government fortifies the system, the community publicizes policy adjustments, and its staff aids patients in insurance procedures and clarifies doubts, ensuring patients fully enjoy benefits and utilize resources. Through the combined efforts of government policies and community cooperation in occupation, income, and insurance aspects, the impact of socio-economic factors on the healthy lifestyle of elderly diabetic patients can be narrowed, enhancing their overall health and safeguarding their rights.
Strengths and weaknesses of the study
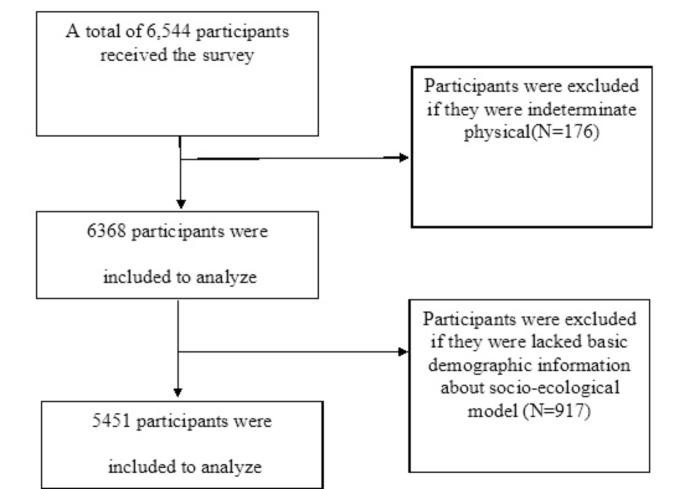
This study systematically examined the factors influencing healthy lifestyles among older adults with diabetes in rural areas, offering several notable strengths. First, it was conducted in a representative county in China, providing a comprehensive survey of all individuals aged 65 and above. The large sample size enhances the credibility and generalizability of the findings within similar contexts. Second, the study incorporated complex and in-depth indicators, offering valuable insights into the multifaceted factors affecting healthy lifestyles in this population. These strengths contribute to a robust foundation for understanding lifestyle determinants in rural elderly populations.
However, the study also has few limitations. First, its cross-sectional design precludes causal inferences between healthy lifestyles and associated factors, limiting the strength of evidence and requiring careful interpretation and application of the results. Second, this study employed whole-cluster sampling and was a single-center study centered in a county. The research findings may be highly applicable to similar administrative units. However, the research results may be subject to selection bias, which restricts the generalizability of the findings and affects the applicability to a broader population. While the results provide useful guidance at the county level, extending these conclusions to larger regions, such as provinces or the entire country, warrants further research and validation. Third, the socioecological model offers an edge in multifaceted factor consideration. However, its limitations, including factor independence presumption and exclusion of some potential aspects, may affect result interpretation and conclusion generality, necessitating optimization or integration of other methods in future research. Fourth, the study relied on self-reported data. This could introduce potential biases as participants might inaccurately report their behaviors due to factors like inaccurate memory or social desirability, thereby affecting the reliability of the data and, to some extent, the accuracy of the research conclusions. Finally, the discussion at the policy level was only focused on the types of medical insurance and did not fully consider other policy factors that might affect the healthy lifestyle of older adults with diabetes. Future research that comprehensively considers more policy factors would be beneficial for constructing a more comprehensive policy intervention framework.