Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. 2017;135:e146–603.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74:2529–32.
Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks: a compass for global action. J Am Coll Cardiol. 2020;76:2980–1.
Griggs D, Stafford-Smith M, Gaffney O, Rockström J, Ohman MC, Shyamsundar P, et al. Policy: sustainable development goals for people and planet. Nature. 2013;495:305–7.
Lee SH, Park SY, Choi CS. Insulin resistance: from mechanisms to therapeutic strategies. Diabetes Metab J. 2022;46:15–37.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10:293–302.
Gast KB, Tjeerdema N, Stijnen T, Smit JW, Dekkers OM. Insulin resistance and risk of incident cardiovascular events in adults without diabetes: meta-analysis. PLoS ONE. 2012;7:e52036.
Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. 2021;119:154766.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122.
Wu H, Ballantyne CM. Metabolic inflammation and insulin resistance in obesity. Circ Res. 2020;126:1549–64.
Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294:E15–26.
NCD Risk Factor Collaboration (NCD-RisC). Global variation in diabetes diagnosis and prevalence based on fasting glucose and hemoglobin A1c. Nat Med. 2023;29:2885–901.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6:299–304.
Ramdas Nayak VK, Satheesh P, Shenoy MT, Kalra S. Triglyceride glucose (TyG) index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. 2022;72:986–8.
Raimi TH, Dele-Ojo BF, Dada SA, Fadare JO, Ajayi DD, Ajayi EA, et al. Triglyceride-glucose index and related parameters predicted metabolic syndrome in Nigerians. Metab Syndr Relat Disord. 2021;19:76–82.
Lim J, Kim J, Koo SH, Kwon GC. Comparison of triglyceride glucose index, and related parameters to predict insulin resistance in Korean adults: an analysis of the 2007–2010 Korean National health and nutrition examination survey. PLoS ONE. 2019;14:e0212963.
Park HM, Lee HS, Lee YJ, Lee JH. The triglyceride-glucose index is a more powerful surrogate marker for predicting the prevalence and incidence of type 2 diabetes mellitus than the homeostatic model assessment of insulin resistance. Diabetes Res Clin Pract. 2021;180:109042.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95:3347–51.
Cui C, Qi Y, Song J, Shang X, Han T, Han N, et al. Comparison of triglyceride glucose index and modified triglyceride glucose indices in prediction of cardiovascular diseases in middle aged and older Chinese adults. Cardiovasc Diabetol. 2024;23:185.
Dang K, Wang X, Hu J, Zhang Y, Cheng L, Qi X, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003–2018. Cardiovasc Diabetol. 2024;23:8.
Miao H, Zhou Z, Yang S, Zhang Y. The association of triglyceride-glucose index and related parameters with hypertension and cardiovascular risk: a cross-sectional study. Hypertens Res. 2024;47:877–86.
Zhuang Y, Qiu L, Han D, Qiao Z, Wang F, Jiang Q, et al. The association between triglyceride-glucose index and related parameters and risk of cardiovascular disease in American adults under different glucose metabolic states. Diabetol Metab Syndr. 2024;16:102.
Park HM, Han T, Heo SJ, Kwon YJ. Effectiveness of the triglyceride-glucose index and triglyceride-glucose-related indices in predicting cardiovascular disease in middle-aged and older adults: a prospective cohort study. J Clin Lipidol. 2024;18:e70–9.
Liu L, Peng J, Wang N, Wu Z, Zhang Y, Cui H, et al. Comparison of seven surrogate insulin resistance indexes for prediction of incident coronary heart disease risk: a 10-year prospective cohort study. Front Endocrinol (Lausanne). 2024;15:1290226.
Ahn SH, Lee HS, Lee JH. Triglyceride-glucose-waist circumference index predicts the incidence of cardiovascular disease in Korean populations: competing risk analysis of an 18-year prospective study. Eur J Med Res. 2024;29:214.
Ren Q, Huang Y, Liu Q, Chu T, Li G, Wu Z. Association between triglyceride glucose-waist height ratio index and cardiovascular disease in middle-aged and older Chinese individuals: a nationwide cohort study. Cardiovasc Diabetol. 2024;23:247.
Li S, An L, Fu Z, Zhang W, Liu H. Association between triglyceride-glucose related indices and all-cause and cause-specific mortality in the general population: a cohort study. Cardiovasc Diabetol. 2024;23:286.
Zhu X, Xu W, Song T, Wang X, Wang Q, Li J, et al. Changes in the combination of the triglyceride-glucose index and obesity indicators estimate the risk of cardiovascular disease. Cardiovasc Diabetol. 2024;23:192.
Xia X, Chen S, Tian X, Xu Q, Zhang Y, Zhang X, et al. Association of triglyceride-glucose index and its related parameters with atherosclerotic cardiovascular disease: evidence from a 15-year follow-up of Kailuan cohort. Cardiovasc Diabetol. 2024;23:208.
Papakonstantinou E, Oikonomou C, Nychas G, Dimitriadis GD. Effects of diet, lifestyle, chrononutrition and alternative dietary interventions on postprandial glycemia and insulin resistance. Nutrients. 2022;14.
Mikusova V, Mikus J, Grilusova K, Roncakova M, Benko J, Martinka E. Insulin resistance and need for a lifestyle change to eliminate it. Bratisl Lek Listy. 2021;122:567–71.
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20:12.
Valenzuela PL, Carrera-Bastos P, Gálvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM, et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. 2021;18:251–75.
Kaminsky LA, German C, Imboden M, Ozemek C, Peterman JE, Brubaker PH. The importance of healthy lifestyle behaviors in the prevention of cardiovascular disease. Prog Cardiovasc Dis. 2022;70:8–15.
Yang J, Christophi CA, Farioli A, Baur DM, Moffatt S, Zollinger TW, et al. Association between push-up exercise capacity and future cardiovascular events among active adult men. JAMA Netw Open. 2019;2:e188341.
Lobelo F, Rohm Young D, Sallis R, Garber MD, Billinger SA, Duperly J, et al. Routine assessment and promotion of physical activity in healthcare settings: A scientific statement from the American heart association. Circulation. 2018;137:e495–522.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting National goals for cardiovascular health promotion and disease reduction: the American heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613.
Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American heart association’s construct of cardiovascular health: a presidential advisory from the American heart association. Circulation. 2022;146:e18–43.
Sun J, Li Y, Zhao M, Yu X, Zhang C, Magnussen CG, et al. Association of the American heart association’s new life’s essential 8 with all-cause and cardiovascular disease-specific mortality: prospective cohort study. BMC Med. 2023;21:116.
Yi J, Wang L, Guo X, Ren X. Association of life’s essential 8 with all-cause and cardiovascular mortality among US adults: a prospective cohort study from the NHANES 2005–2014. Nutr Metab Cardiovasc Dis. 2023;33:1134–43.
Xing A, Tian X, Wang Y, Chen S, Xu Q, Xia X, et al. Life’s essential 8’ cardiovascular health with premature cardiovascular disease and all-cause mortality in young adults: the Kailuan prospective cohort study. Eur J Prev Cardiol. 2023;30:593–600.
Zhang J, Chen G, Habudele Z, Wang X, Cai M, Li H, et al. Relation of life’s essential 8 to the genetic predisposition for cardiovascular outcomes and all-cause mortality: results from a National prospective cohort. Eur J Prev Cardiol. 2023;30:1676–85.
Rempakos A, Prescott B, Mitchell GF, Vasan RS, Xanthakis V. Association of life’s essential 8 with cardiovascular disease and mortality: the Framingham heart study. J Am Heart Assoc. 2023;12:e030764.
Sebastian SA, Shah Y, Paul H, Arsene C. Life’s Essential 8 and the risk of cardiovascular disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2024.
Isiozor NM, Kunutsor SK, Voutilainen A, Laukkanen JA. Life’s essential 8 and the risk of cardiovascular disease death and all-cause mortality in Finnish men. Eur J Prev Cardiol. 2023;30:658–67.
Wang L, Xie J, Hu Y, Tian Y. Air pollution and risk of chronic obstructed pulmonary disease: the modifying effect of genetic susceptibility and lifestyle. EBioMedicine. 2022;79:103994.
Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. N Engl J Med. 2020;383:49–57.
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, et al. Association between wait time and 30-Day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994–2003.
Kim MS, Shim I, Fahed AC, Do R, Park WY, Natarajan P, et al. Association of genetic risk, lifestyle, and their interaction with obesity and obesity-related morbidities. Cell Metab. 2024;36:1494–e15031493.
Yucel RM. State of the multiple imputation software. J Stat Softw. 2011;45.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Bruckner F, Gruber JR, Ruf A, Edwin Thanarajah S, Reif A, Matura S. Exploring the link between lifestyle, inflammation, and insulin resistance through an improved healthy living index. Nutrients. 2024;16.
Hivert MF, Christophi CA, Franks PW, Jablonski KA, Ehrmann DA, Kahn SE, et al. Lifestyle and metformin ameliorate insulin sensitivity independently of the genetic burden of established insulin resistance variants in diabetes prevention program participants. Diabetes. 2016;65:520–6.
Towfighi A. Insulin resistance, obesity, metabolic syndrome, and lifestyle modification. Continuum (Minneap Minn). 2011;17:1293–303.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Molavizadeh D, Cheraghloo N, Tohidi M, Azizi F, Hadaegh F. The association between index-year, average, and variability of the triglyceride-glucose index with health outcomes: more than a decade of follow-up in Tehran lipid and glucose study. Cardiovasc Diabetol. 2024;23:321.
Hu B, Wang Y, Wang Y, Feng J, Fan Y, Hou L. Association between triglyceride-glucose index and risk of all-cause and cardiovascular mortality in adults with prior cardiovascular disease: a cohort study using data from the US National health and nutrition examination survey, 2007–2018. BMJ Open. 2024;14:e084549.
Alavi Tabatabaei G, Mohammadifard N, Rafiee H, Nouri F, Maghami Mehr A, Najafian J, et al. Association of the triglyceride glucose index with all-cause and cardiovascular mortality in a general population of Iranian adults. Cardiovasc Diabetol. 2024;23:66.
Lee JH, Jeon S, Lee HS, Lee JW. Trajectories of triglyceride-glucose index changes and their association with all-cause and cardiovascular mortality: a competing risk analysis. Cardiovasc Diabetol. 2024;23:364.
Ke J, Ruan X, Liu W, Liu X, Wu K, Qiu H, et al. Prospective cohort studies underscore the association of abnormal glycemic measures with all-cause and cause-specific mortalities. iScience. 2024;27:110233.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, et al. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21:124.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. Bmj-Brit Med J. 2020;370:m3324.
Salas-Salvadó J, Díaz-López A, Ruiz-Canela M, Basora J, Fitó M, Corella D, et al. Effect of a lifestyle intervention program with energy-restricted mediterranean diet and exercise on weight loss and cardiovascular risk factors: one-year results of the PREDIMED-Plus trial. Diabetes Care. 2019;42:777–88.
Manoogian ENC, Wilkinson MJ, O’Neal M, Laing K, Nguyen J, Van D, et al. Time-restricted eating in adults with metabolic syndrome: a randomized controlled trial. Ann Intern Med. 2024;177:1462–70.
Gong Q, Zhang P, Wang J, Ma J, An Y, Chen Y, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing diabetes prevention outcome study. Lancet Diabetes Endocrinol. 2019;7:452–61.
Effects of Intensive Lifestyle Intervention on All-Cause. Mortality in older adults with type 2 diabetes and overweight/obesity: results from the look AHEAD study. Diabetes Care. 2022;45:1252–9.
Lee CG, Heckman-Stoddard B, Dabelea D, Gadde KM, Ehrmann D, Ford L, et al. Effect of metformin and lifestyle interventions on mortality in the diabetes prevention program and diabetes prevention program outcomes study. Diabetes Care. 2021;44:2775–82.
Reynolds AN, Akerman AP, Mann J. Dietary fibre and whole grains in diabetes management: systematic review and meta-analyses. PLoS Med. 2020;17:e1003053.
Sun D, Man W, Zhang L. Roles of insulin resistance, endothelial dysfunction and lifestyle changes in the development of cardiovascular disease in diabetic patients. Curr Drug Targets. 2017;18:1792–9.
Kaar JL, Simon SL, Schmiege SJ, Nadeau KJ, Kelsey MM. Adolescent’s health behaviors and risk for insulin resistance: a review of the literature. Curr Diab Rep. 2017;17:49.
Rosenberg DE, Jabbour SA, Goldstein BJ. Insulin resistance, diabetes and cardiovascular risk: approaches to treatment. Diabetes Obes Metab. 2005;7:642–53.
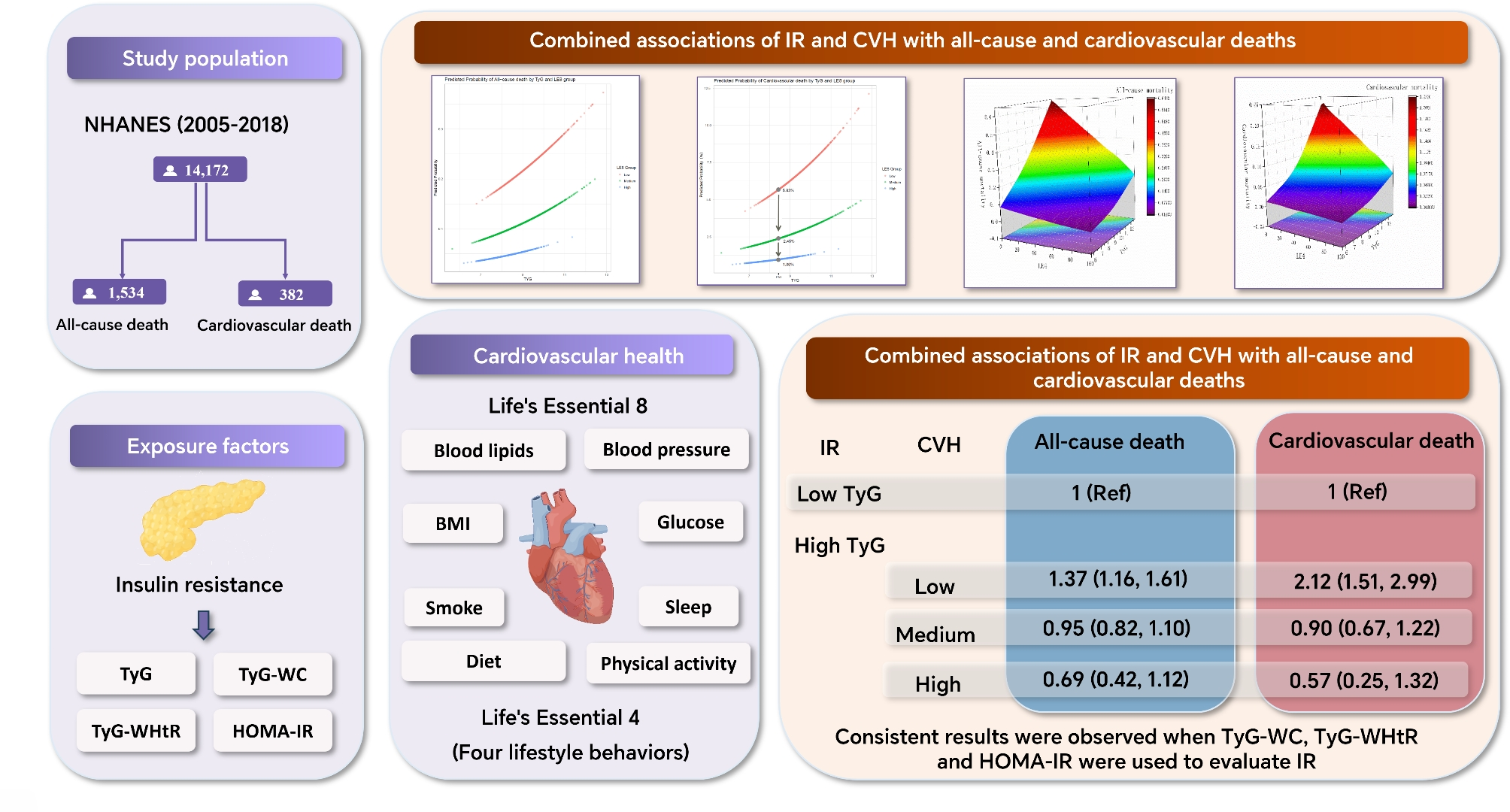
Feng Y, Lin H, Tan H, Liu X. Life’s essential 8 metrics and mortality outcomes in insulin resistance: the role of inflammation, vascular aging, and gender. Clin Nutr ESPEN. 2024;61:131–9.
Hellgren MI, Daka B, Jansson PA, Lindblad U, Larsson CA. Insulin resistance predicts early cardiovascular morbidity in men without diabetes mellitus, with effect modification by physical activity. Eur J Prev Cardiol. 2015;22:940–9.
Helmink MAG, de Vries M, Visseren FLJ, de Ranitz WL, de Valk HW, Westerink J. Insulin resistance and risk of vascular events, interventions and mortality in type 1 diabetes. Eur J Endocrinol. 2021;185:831–40.
Nelson RK, Horowitz JF. Acute exercise ameliorates differences in insulin resistance between physically active and sedentary overweight adults. Appl Physiol Nutr Metab. 2014;39:811–8.
Martins FO, Conde SV. Impact of diet composition on insulin resistance. Nutrients. 2022;14.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Mirabelli M, Chiefari E, Arcidiacono B, Corigliano DM, Brunetti FS, Maggisano V et al. Mediterranean diet nutrients to turn the tide against insulin resistance and related diseases. Nutrients. 2020;12.
Malin SK, Huang H, Mulya A, Kashyap SR, Kirwan JP. Lower dipeptidyl peptidase-4 following exercise training plus weight loss is related to increased insulin sensitivity in adults with metabolic syndrome. Peptides. 2013;47:142–7.
Koren D, Taveras EM. Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metabolism. 2018;84:67–75.
Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56–66.
Bajaj M. Nicotine and insulin resistance: when the smoke clears. Diabetes. 2012;61:3078–80.
Fu J, Liu Y, Zhang L, Zhou L, Li D, Quan H, et al. Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. J Am Heart Assoc. 2020;9:e16804.
Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and control of hypertension: JACC health promotion series. J Am Coll Cardiol. 2018;72:1278–93.
Goldberg L, Elliot DL. The effect of exercise on lipid metabolism in men and women. Sports Med. 1987;4:307–21.
Clifton PM. Diet, exercise and weight loss and dyslipidaemia. Pathology. 2019;51:222–6.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/american heart association task force on clinical practice guidelines. Circulation. 2019;140:e596–646.
Hergesell K, Paraskevopoulou A, Opálka L, Velebný V, Vávrová K, Dolečková I. The effect of long-term cigarette smoking on selected skin barrier proteins and lipids. Sci Rep. 2023;13:11572.
Moradinazar M, Pasdar Y, Najafi F, Shahsavari S, Shakiba E, Hamzeh B, et al. Association between dyslipidemia and blood lipids concentration with smoking habits in the Kurdish population of Iran. BMC Public Health. 2020;20:673.
Zhan Y, Chen R, Yu J. Sleep duration and abnormal serum lipids: the China health and nutrition survey. Sleep Med. 2014;15:833–9.
Juárez-Flores DL, Ezquerra M, Gonzàlez-Casacuberta Ï, Ormazabal A, Morén C, Tolosa E et al. Disrupted mitochondrial and metabolic plasticity underlie comorbidity between age-related and degenerative disorders as Parkinson disease and type 2 diabetes mellitus. Antioxidants-Basel. 2020;9.
Wculek SK, Forisch S, Miguel V, Sancho D. Metabolic homeostasis of tissue macrophages across the lifespan. Trends Endocrin Met. 2024;35:793–808.
Lawrenson L, Hoff J, Richardson RS. Aging attenuates vascular and metabolic plasticity but does not limit improvement in muscle VO(2) max. Am J Physiol-Heart C. 2004;286:H1565–72.
Meyer MR, Clegg DJ, Prossnitz ER, Barton M. Obesity, insulin resistance and diabetes: sex differences and role of oestrogen receptors. Acta Physiol. 2011;203:259–69.
Davis SR, Lambrinoudaki I, Lumsden M, Mishra GD, Pal L, Rees M, et al. Menopause Nat Rev Dis Primers. 2015;1:15004.
Hellsten Y. Oestrogen, exercise and vascular function. J Physiol. 2019;597:4871.